“If it’s not recorded, it didn’t happen.” – An old saying We wanted to find out how much teaching on addiction get on medical students. In 2011,
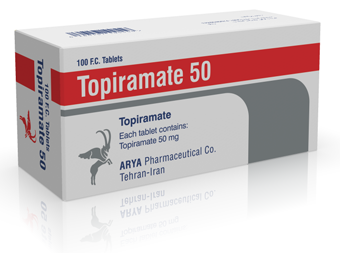
How can we do better job in studying Topiramate?
Topiramate prevents seizures in people with epilepsy. Previously, we looked at all studies to see whether Topiramate can help treat cocaine addiction,
New review out now: Epilepsy drug fails crack addiction
This review asked whether a drug for epilepsy seizures – Topiramate - can help treat cocaine addiction, reduce cocaine use and prolong treatment
Reducing drinking in illicit drug users: an impact story @COMETinitiative
Research impact is often hard to prove. It takes years before our findings change the world and the change is often small. This new abstract
Alcohol and Methadone Don’t Mix! What’s New in Addiction Medicine? lecture series
Please join us on Tuesday, October 27 for this month’s edition of the “What’s New in Addiction Medicine?” lecture series. This (free) event
Health care research is untidy – what does it mean for postdocs? #CochraneCalgary2015
Why do we study health? Because we want to help patients. It’s no rocket science. And yet, most clinical trials do not measure outcomes that are
How Cochrane Keeps the Addiction Science in Check
Science isn’t infallible. Humans make mistakes even in this highly sophisticated method of understanding the world around us. Thanks God, addiction
Finding the Evidence for Talking Therapies: Article in the Forum magazine
In an attempt to prove that counseling works for reducing drinking in concurrent problem alcohol and illicit drug users, I ended up on a journey
How to go about getting a postdoc position? Finding funding
There probably isn’t a simple answer to this question. Everybody has a different experience. My path was one of finding my own funding to do what I