In a new article from the Academic Medicine, we argue that clinician-scientist training is one of the most important bridges to cross the growing
6 ways to improve addiction training
Addiction training is feasible and acceptable for doctors and junior physicians; however, important barriers persist. We need to learn more about the
Nursing Fellowship in Addiction Medicine
Traditionally, nursing and physician education have been separated through separate programmes despite working closely together in real-world
Better medical education: One solution to the opioid crisis
Opioid overdose is a complex problem, no one solution is the best. But effective interventions can help manage opioid addiction. Yet, many effective
What are the core skills of an addiction expert?
Should all medical doctors receive the same training in addiction medicine? Here's what international experts think about core skills of and addiction
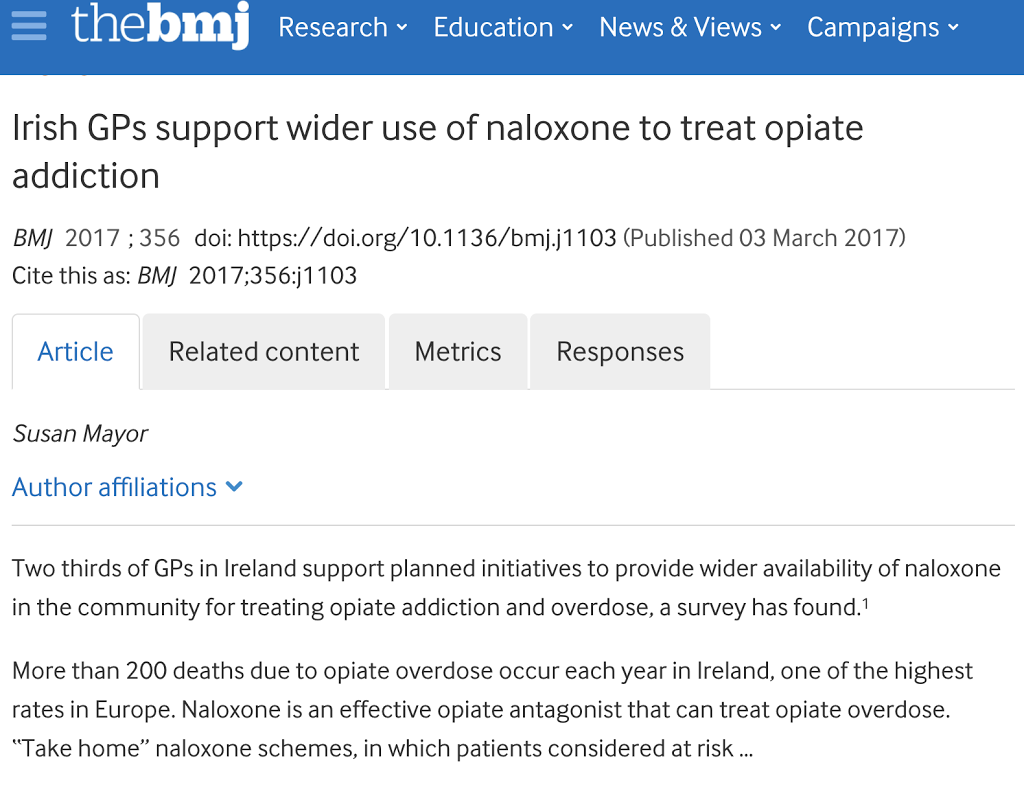
Irish GPs support wider use of naloxone to treat opiate addiction
Two thirds of GPs in Ireland support planned initiatives to provide wider availability of naloxone in the community for treating opiate addiction and
Insite Inside Out
Insite, "is that the place where people shoot up heroin? Do you shoot heroin?" a border officer asked me when he saw the sign on my T-shirt. I was
How can we do better job in studying Topiramate?
Topiramate prevents seizures in people with epilepsy. Previously, we looked at all studies to see whether Topiramate can help treat cocaine addiction,
Changing the ways of CPDD – College on Problems of Drug Dependence – June 12-16, #CPDD2016
Change is the ultimate law of life. Those that do not change and adapt, do not survive. In the life of scientific meetings, this means constantly