Connecting professionals can promote interdisciplinary trauma-focused therapy and return-to-work support for clients with work-related PTSD. This blog
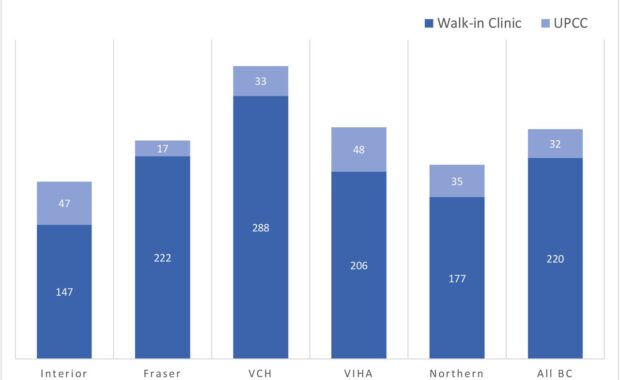
Comparing Walk-in Clinics and Urgent Primary Care Centers
Walk-in clinics are non-hospital based primary care facilities that are designed to operate without appointments and provide increased healthcare
Group therapy alleviates psychological distress in prostate cancer
Emerging evidence that group therapy helps men with prostate cancer.
Dennis McCarty receives prestigious Kentucky award 2022
Dennis McCarty, Ph.D., an Emeritus Professor in the School of Public Health at the Portland State University and Oregon Health & Science
Why inequality hinders effective pain relief for opioid naive people
Equitable access to care is problematic; some people get it, most are left out. The REDONNA study (https://doi.org/10.1016/j.cct.2021.106462) began
Finding 1239 primary care clinics using license registry algorithm
Some Canadians have limited access to longitudinal primary care, despite its known advantages for population health. Current initiatives to transform
Can online training uplift opioid sparing strategies?
Opioid analgesic prescribing has been in trouble for decades in North America. Things are changing, though. Still, there’s room to adjust care,
Exploring barriers and facilitators to health equity
[April 27] The ongoing opioid crisis continues to inflict serious harms on thousands of British Columbians. Some harms are due to initiation of opioid
Where science meets meditative solutions
Tired, overwhelmed, or stressed out? Worried about the future and what it may bring? Then join us for the Spring Session of an 8 week meditation