Shifting focus on accelerating innovative solutions and clarifying roles can help reduce unregulated drug deaths. Bardwell and colleagues(1)
I’m almost opioid-a-phobic: Family medicine residents perceive
Over the past two decades, Canadians’ use of opioid analgesics has substantially grown, making the nation the second-largest user of opioid analgesics
Filling the substance use treatment gap requires better education and research training
While education is unlikely the ultimate filling for the substance use treatment gap, it is one that can be hardly overlooked and
Can online training uplift opioid sparing strategies?
Opioid analgesic prescribing has been in trouble for decades in North America. Things are changing, though. Still, there’s room to adjust care,
Exploring barriers and facilitators to health equity
[April 27] The ongoing opioid crisis continues to inflict serious harms on thousands of British Columbians. Some harms are due to initiation of opioid
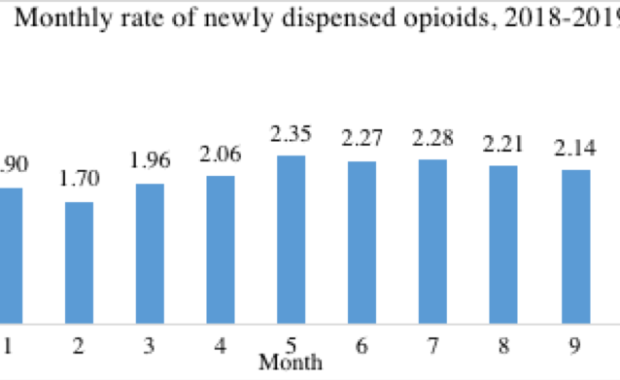
Newly started primary care opioid prescriptions plateaued in 2018-2019
Our new study published in the Canadian Journal of Addiction found plateauing rates of new starts of opioid analgesics in British Columbia in
Can intentional substance use reduce illicit opioid use?
Have you ever intentionally used an alternate substance to control or reduce your use of illicit (non-prescribed) opioids? Self-managed use is one
This changed my practice
Can We Identify Patients at Risk for Opioid Use Disorder when Beginning Opioid Analgesics for Pain from New or Ongoing Non-cancer Causes? There is
Male Pain and Alcohol
Pain is a universal experience across people of all genders. How do we know when something hurts inside? It keeps coming back; first, it disrupts,