Walk-in clinics are non-hospital based primary care facilities that are designed to operate without appointments and provide increased healthcare
Group therapy alleviates psychological distress in prostate cancer
Emerging evidence that group therapy helps men with prostate cancer.
Filling the substance use treatment gap requires better education and research training
While education is unlikely the ultimate filling for the substance use treatment gap, it is one that can be hardly overlooked and
How can people with opioid use disorder get better virtual care?
Virtual care is the new normal around the globe. The emergence of COVID-19 introduced a dual public health emergency in British Columbia. The province
Why inequality hinders effective pain relief for opioid naive people
Equitable access to care is problematic; some people get it, most are left out. The REDONNA study (https://doi.org/10.1016/j.cct.2021.106462) began
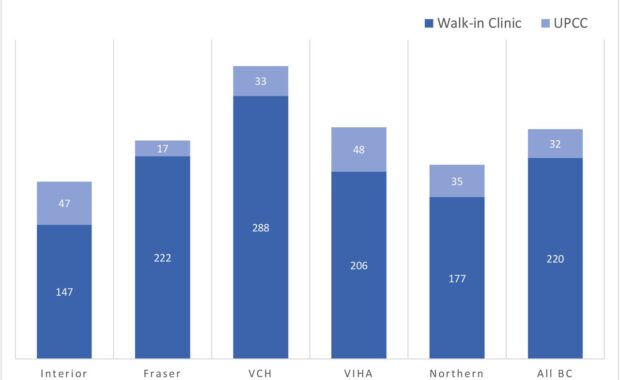
Finding 1239 primary care clinics using license registry algorithm
Some Canadians have limited access to longitudinal primary care, despite its known advantages for population health. Current initiatives to transform
Mentoring helps physicians publish more peer-reviewed papers, study says
Physician scientists help advance the science of addiction medicine, yet prior studies have not looked at better ways of increasing publication
Hospital based opioid agonist treatment
Researchers recently found that many people with co-occurring mental health and substance use disorders are admitted to inpatient psychiatric units.
Excellent scale assesses needs across four countries
What is the smartest scale for asking clinicians about their training needs? In a new article published by the Journal of Substance Abuse