Shifting focus on accelerating innovative solutions and clarifying roles can help reduce unregulated drug deaths. Bardwell and colleagues(1)
Why inequality hinders effective pain relief for opioid naive people
Equitable access to care is problematic; some people get it, most are left out. The REDONNA study (https://doi.org/10.1016/j.cct.2021.106462) began
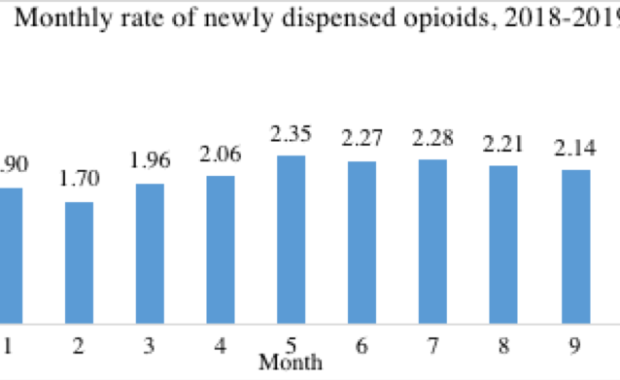
Newly started primary care opioid prescriptions plateaued in 2018-2019
Our new study published in the Canadian Journal of Addiction found plateauing rates of new starts of opioid analgesics in British Columbia in
Hospital based opioid agonist treatment
Researchers recently found that many people with co-occurring mental health and substance use disorders are admitted to inpatient psychiatric units.
Why most opioid risk tools fail?
How many of you had a flu this winter? Anyone took antibiotics for that? But some people can’t take them because they are allergic. Now, imagine
Training medical students in addiction medicine can help in the opioid crisis
Better medical education is one solution to the opioid overdose crisis, but our new study suggests that few students have direct experience of
Lisbon conference reviews addiction literature
What is the state of the art in addiction research? How do we measure recovery? These, and other questions dominated presentations on systematic
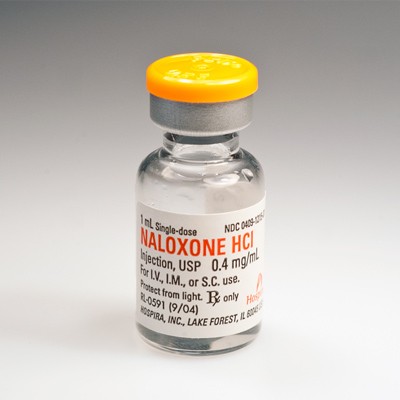
Families of opioid users in Ireland may be given drug to stop overdose deaths
By Siobhan MaguireArticle from The Sunday Times, 21 September 2014, p4The department of healthis reviewing distribution of Naloxone, a drug that
Overdose Education and Naloxone: Workshop for Family Medicine Trainees in Ireland
Overdose is the most common cause of deaths among heroin users. Our previous research has shown that the ambulances in Dublin see one overdose every