Connecting professionals can promote interdisciplinary trauma-focused therapy and return-to-work support for clients with work-related PTSD. This blog
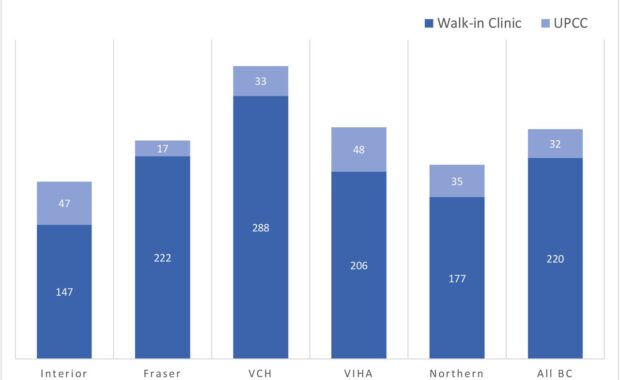
Comparing Walk-in Clinics and Urgent Primary Care Centers
Walk-in clinics are non-hospital based primary care facilities that are designed to operate without appointments and provide increased healthcare
I’m almost opioid-a-phobic: Family medicine residents perceive
Over the past two decades, Canadians’ use of opioid analgesics has substantially grown, making the nation the second-largest user of opioid analgesics
Filling the substance use treatment gap requires better education and research training
While education is unlikely the ultimate filling for the substance use treatment gap, it is one that can be hardly overlooked and
Why inequality hinders effective pain relief for opioid naive people
Equitable access to care is problematic; some people get it, most are left out. The REDONNA study (https://doi.org/10.1016/j.cct.2021.106462) began
Family physician and practice characteristics in audit and feedback
Audit and feedback interventions elicit behaviour change by describing existing patterns of behaviour and providing education about desired ideal
Can online training uplift opioid sparing strategies?
Opioid analgesic prescribing has been in trouble for decades in North America. Things are changing, though. Still, there’s room to adjust care,
Exploring barriers and facilitators to health equity
[April 27] The ongoing opioid crisis continues to inflict serious harms on thousands of British Columbians. Some harms are due to initiation of opioid
Mentoring helps physicians publish more peer-reviewed papers, study says
Physician scientists help advance the science of addiction medicine, yet prior studies have not looked at better ways of increasing publication