Shifting focus on accelerating innovative solutions and clarifying roles can help reduce unregulated drug deaths. Bardwell and colleagues(1)
Why inequality hinders effective pain relief for opioid naive people
Equitable access to care is problematic; some people get it, most are left out. The REDONNA study (https://doi.org/10.1016/j.cct.2021.106462) began
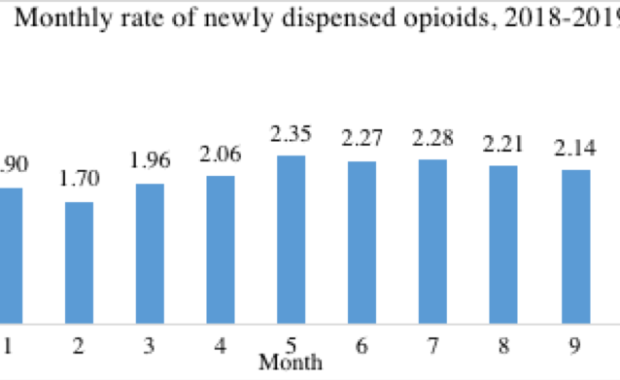
Newly started primary care opioid prescriptions plateaued in 2018-2019
Our new study published in the Canadian Journal of Addiction found plateauing rates of new starts of opioid analgesics in British Columbia in
Can intentional substance use reduce illicit opioid use?
Have you ever intentionally used an alternate substance to control or reduce your use of illicit (non-prescribed) opioids? Self-managed use is one
Thrive supports caregivers coping with family substance use issues
Thrive is a supportive network for family and friend caregivers of older adults who use substances or alcohol.Authors: Michee-Ana Hamilton, MSc and
Moving on: helping young people
In this 2009 Insight article, Gemma Turner, Cobh Community Based Drugs Worker, provides a brief history of the project while Jano Klimas gives a sense
Expanding opioid agonist therapy while learning from HIV/AIDS
Accessing opioid agonist therapy (OAT) and maintaining good adherence faces many barriers which can be geographical, financial, regulatory,
Hospital based opioid agonist treatment
Researchers recently found that many people with co-occurring mental health and substance use disorders are admitted to inpatient psychiatric units.
America could relax opioid treatment access policies
Canada and the United States (U.S.) face an opioid use disorder and opioid overdose epidemic. The most effective OUD treatment is opioid agonist