There has been a noticeable deficiency in the implementation of addiction science in healthcare practice. Many physicians and healthcare providers
Moving on: helping young people
In this 2009 Insight article, Gemma Turner, Cobh Community Based Drugs Worker, provides a brief history of the project while Jano Klimas gives a sense
Towards a research agenda for addiction education in Europe, u21 poster
u21 health sciences group 2020 virtual meeting: A collaborative approach to healthcare was hosted by University College Dublin from August 25th -
How to find non-academic mentors
Mentors facilitate professional development in academia. But non-academic mentors are equally important. Here, I acknowledge non-academic mentors and
Can Community First Responders reverse Cardiac arrests?
Out-of-hospital cardiac arrest is a major cause of death. It occurs when a person’s heart stops pumping blood around the body. It is most often caused
Off the record: addictions in medical schools
“If it’s not recorded, it didn’t happen.” – An old saying We wanted to find out how much teaching on addiction get on medical students. In 2011,
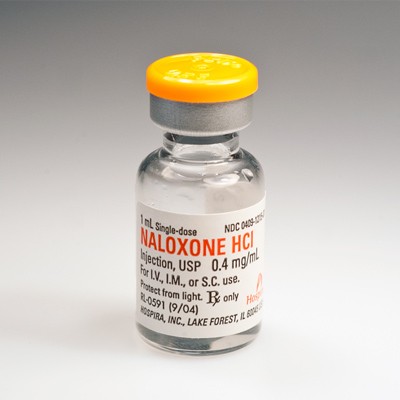
General practice is a key route for distribution of naloxone in the community
Naloxone is an antidote to opioid overdose also known as Narcan. Irish family doctors in training want Narcan to be more available and want to
What do persons on methadone in primary care think about alcohol screening?
Enhancing alcohol screening and brief intervention among people receiving opioid agonist treatment: Qualitative study in primary care New Paper Out
Recipe for untangling complex healthcare
So there he was, with the boy's head in his hands. The boy was 12, but looked no more than 10 years old. He was deeply jaundiced and in a heroin