Connecting professionals can promote interdisciplinary trauma-focused therapy and return-to-work support for clients with work-related PTSD. This blog
Group therapy alleviates psychological distress in prostate cancer
Emerging evidence that group therapy helps men with prostate cancer.
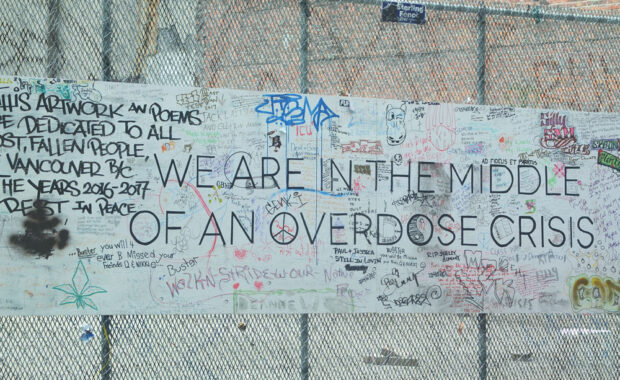
How can people with opioid use disorder get better virtual care?
Virtual care is the new normal around the globe. The emergence of COVID-19 introduced a dual public health emergency in British Columbia. The province
Dennis McCarty receives prestigious Kentucky award 2022
Dennis McCarty, Ph.D., an Emeritus Professor in the School of Public Health at the Portland State University and Oregon Health & Science
This changed my practice
Can We Identify Patients at Risk for Opioid Use Disorder when Beginning Opioid Analgesics for Pain from New or Ongoing Non-cancer Causes? There is
Hospital based opioid agonist treatment
Researchers recently found that many people with co-occurring mental health and substance use disorders are admitted to inpatient psychiatric units.
Boost for Oral Opioid Agonist Therapy
Although opioid agonist treatment is effective in treating opioid use disorders, retention in such treatment is suboptimal in part due to quality of
Why most opioid risk tools fail?
How many of you had a flu this winter? Anyone took antibiotics for that? But some people can’t take them because they are allergic. Now, imagine
Hospital teaching team keeps fighting opioid crisis
Which student learns best with hospital teams fighting opioid crisis? Understanding how students learn is perhaps the most important way to improve