Although opioid agonist treatment is effective in treating opioid use disorders, retention in such treatment is suboptimal in part due to quality of
Why most opioid risk tools fail?
How many of you had a flu this winter? Anyone took antibiotics for that? But some people can’t take them because they are allergic. Now, imagine
Place matters, teachers and learners #CCME18
We learn best in places that support our learning and our bio psycho socio spiritual development – from toddlers to elders, reports Jan Klimas from
Does alcohol use change after shift to Methadose?
Do people drink more when they switch to Methadose? It is 10 times more concentrated than methadone - proven treatment of opioid use disorder. We did
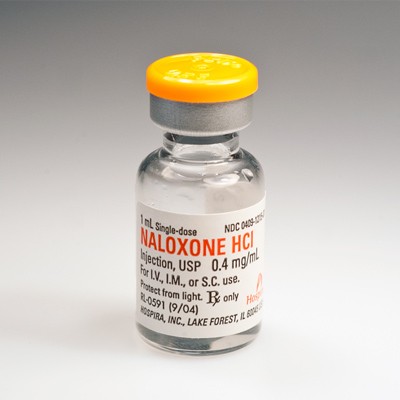
Naloxone and Irish Primary Care Practitioners
We wanted to know what General Practitioners’ (GP) views and experiences of opioid addiction, overdose care and naloxone provision are. Naloxone is an
Hospital teaching teams confront iatrogenic opioid addiction
What can hospital teams teach medical students about addiction to help curb the opioid overdose epidemic? In a new article published by the
Two birds with one stone: physicians training in research
Combined training in addiction medicine and research is feasible and acceptable for physicians - a new study shows; however, there are important
General practice is a key route for distribution of naloxone in the community
Naloxone is an antidote to opioid overdose also known as Narcan. Irish family doctors in training want Narcan to be more available and want to
What do persons on methadone in primary care think about alcohol screening?
Enhancing alcohol screening and brief intervention among people receiving opioid agonist treatment: Qualitative study in primary care New Paper Out